Abstract
Background Sickle cell disease (SCD) is a genetic disorder of hemoglobin with hemolysis and vaso-occlusion that leads to pain, joint damage, and impairment in physical function. Advancements in care have increased the lifespan of individuals with SCD. Even with improvements in care, there is limited knowledge regarding how to measure and maintain physical activity in adults with SCD. Wearable devices can remotely track physiologic markers of pain in people with SCD and are used in older adults in the general population to track physical activity and health-related outcomes. Despite the popularity of wearable devices, the feasibility of using accelerometers to measure physical activity in older adults with SCD is unknown. The purpose of this study was to assess the feasibility of the Actigraph accelerometer to objectively measure physical activity in adults with SCD.
Methods We enrolled younger adults (age 18-39) and older adults (age ≥ 40 years) with SCD in a prospective cohort study of physical activity using an Actigraph accelerometer. We instructed participants to wear the Actigraph wGT3X-BT or GT9X Link device on their non-dominant wrist for 7 consecutive days during waking hours and to remove it when they showered. If they missed a day of wearing the accelerometer, we asked them to add an additional day to complete 7 days. Activity data was processed in ActiLife Software 6 (ActiGraph, LLC).
We defined feasibility endpoints by the percent of participants who returned the accelerometer and percent of participants who wore it for ≥ 3 days for a least 10 hours/day. We analyzed physical activity by measuring steps per day and proportion of wear time spent being sedentary, doing light activity, and doing moderate-vigorous physical activity (MVPA).
We assessed relationships between physical activity (steps per day), physical performance measures (six-minute walk distance (6MWD), usual gait speed, Timed-Up and Go (TUG), seated grip strength, and 30-second chair stands), and the 36-item Short Form (SF-36) physical functioning.
Results Sixty participants received an accelerometer. Out of these 60 participants, 90% (n=54) returned the accelerometer after 7 days.
Among those who returned accelerometers, the mean age was 43 years (range 19 - 71). The mean age was 26 (range 19-36) for younger adults and 54 (range 40- 71) for older adults. The majority (61%) of participants were older adults. Most (56%) participants were female. Most (56%) had HbSS, 6% HbSβ0-thalassemia, 30% HbSC, and 9% HbSβ+-thalassemia.
On wear time validation, 83% (n=50) of participants wore the monitor for at least 3 days for at least 10 hours per day.
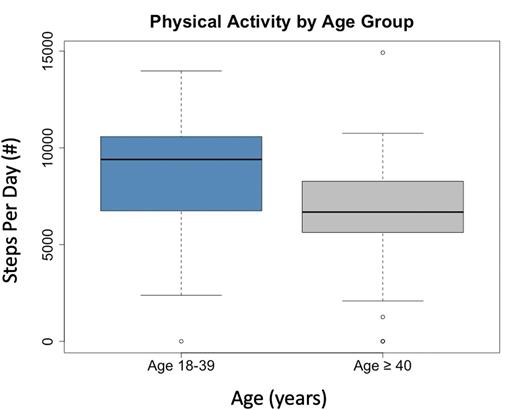
The mean wear time was 7 days (range 0-15 days). The median steps per day for all participants was 7235 (range 0-14916; IQR 5892-9406). The median steps per day for younger adults was 9397 (IQR 6739 - 10578) and 6678 (IQR 5621-8268) for older adults. There was a significant difference in steps per day between younger and older adults (p-value = 0.021).
On average, participants were sedentary 39% (±15%) of the time, doing light activity 45% (±14%) of the time, and MVPA 11% (±6%) of the time. The average daily time spent doing MVPA was 111 minutes (± 66 minutes).
Physical activity (median steps per day) had moderate correlations with the TUG (rs = -0.3; p=0.03), 6MWD (rs = 0.29; p=0.04), 30-second chair stands (rs = 0.32; p=0.02), and SF-36 (rs = 0.34; p=0.036). When we controlled for age, there no longer was a relationship between steps per day and 6MWD (p=0.99) and TUG (p=0.12); however, the positive correlation between step per day and 30-second chair stands remained (p=0.047). Usual gait speed (rs = 0.056; p=0.69) and seated grip strength (rs =0.17; p=0.23) did not correlate with physical activity.
Conclusion The results of the study support accelerometers as a feasible measure of physical activity in younger and older adults with SCD. Most participants wore and were able to return their activity monitors without difficulty. There was a moderate positive correlation between steps per day and physical function that was mostly driven by age. There remained a significant relationship between steps per day and number of chair stands when we controlled for age, which suggests that consistent physical activity may play a role in maintaining lower body strength in adults with SCD. In future studies we will use accelerometers to monitor physical activity in response to geriatric-based interventions for older adults with SCD.
Disclosures
Strouse:Takeda: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal